Introduction
With the exception of the use of thoracoscopy for diagnosis, indications for surgery in mesothelioma are controversial. Due to the rarity of disease there are no randomized surgical studies on which to base objective treatment decisions, and most of what constitutes current guidelines has been based on single center retrospective studies or phase I/II trials with limited numbers of patients. This chapter will examine the role of surgery for diagnosis, staging, palliation, and therapy for MPM. In understanding the currensurgical literature for this disease, the reader is reminded that comparisons between reported series are difficult. Factors that highly influence the outcome such as tumor stage and histology are not only often difficult to accurately define in an individual patient but are often variably documented in published reports. Furthermore, indications for selection of patients to undergo a given procedure are often poorly explained (if at all) and this inevitably leads to bias when comparisons are performed between different series.
Natural History
The natural history of mesothelioma is for the tumor to progress locally causing dyspnea, by either lung entrapment or compression from effusion leading to atelectasis and shunting, and pain from chest wall invasion. Death usually occurs within 6–12 months from initial diagnosis. Though autopsy studies reveal that metastases occur in 50–75% of cases, most are clinically occult and are not the cause of death. The majority
of patients with MPM are diagnosed when the tumor is at an advanced stage. Many untreated patients with early stage disease (American Joint Commission on Cancer (AJCC) Stage I) will probably survive significantly longer than 12 months. Ruffie et al reported median survival of 6.8 months from date of diagnosis until death in 176 untreated patients from 9 Canadian centers from 1969 to 1984. Two more recent trials, however, serve as useful contempoRary benchmarks for outcome in untreated patients. Merritt et al. reported a median survival of 7.1 months in 101 consecutive patients with MPM treated at two tertiary referral centers in Ontario. Symptom management alone was performed. Patients were not clinically staged, and a relatively large proportion (57%) had non-epithelioid tumors, which are
known to have worse outcome. Another trial performed by the Medical Research Council of Great Britain randomized 409 patients to chemotherapy or active symptom control which included use of steroids, appetite stimulants, bronchodilators, or palliative radiotherapy. Epithelioid tumors occurred in 74% of patientsand 79% were AJCC stage III or IV, proportions that are consistent with most clinical series. Median survival calculated from the date of randomization (median 60 days from date of diagnosis) was 7.6 months, and 1-year survival was 29%. Chemotherapy did not have a survival benefit over active symptom control; however, pemetrexed, the current standard chemotherapeutic agent was not included in the drug regimen. Two recent prospective randomized trials using modern platinum/antifolate doublet regimens
showed median survival of 11.4 months and 12.1 months, respectively, in non-resectable patients . The median survival for untreated patients is therefore probably between 7 and 10 months from the date of diagnosis and with chemotherapy may extend to 12–13 months, but will be influenced by initial stage and tumor histology. Though these studies provide a rough benchmark on which to base survival comparisons
with surgical series. One must remember that subjects in most surgical series are usually a highly select group of good performance status patients. The natural history of MPM in such patients is still poorly defined.
Diagnosis
Video-Assisted Thoracoscopy
The benefit of video-assisted thoracoscopic surgery (VATS) for the diagnosis of MPM is that it is a safe, simple, widely available, and highly accurate diagnostic procedure. VATS allows large tissue samples to be obtained from multiple areas of the thoracic cavity, an important consideration since there is considerable
tumor heterogeneity within individual mesothelioma tumors. In fact it has been shown that sarcomatoid elements within a mesothelioma are not uniformly distributed within the tumor and that the greater the number of separate biopsies that are taken, the higher the likelihood of diagnosing biphasic (or mixed) histologic
subtype. As patients with non-epithelioid tumors have significantly worse outcome aftercytoreductive surgery than those with epithelioid tumors do, prior knowledge of cell type can greatly influence subsequent therapy. VATS is generally best performed through a single 1–1.5 cm incision placed on the lateral chest
wall in line of a potential future thoracotomy. The rationale for this is that MPM can occasionally track along thoracostomy incisions, thus limiting the number of incisions that is beneficial and placement in a region that can be completely excised at the time of future cytoreductive surgery facilitates complete resection
without having to perform additional excision of multiple thoracostomy sites. A single 1.5 cm incision will usually allow for placement of a 5 mm angled thoracoscope and an endoscopic biopsy forceps through a soft thoracostomy port. Alternatively, a thoracoscope with a working channel can be used. A single chest drain an subsequently be placed through the same incisio , though it is useful to close the fascia and ubcutaneous tissue around the chest drainto limit postoperative leakage of pleural Fluid. VATS can identify whether tumor involves the visceral pleura as well as the parietal pleura (IMIG/AJCC stage IB) but is otherwise fairly limited as a staging modality. VATS lymphadenectomy is to be avoided as a staging
procedure as the interruption of tissue planes may hamper subsequent cytoreductive surgery and it is prone to false positivity due to contamination of specimens from the surrounding tumor. VATS is most easily performed in patients where a large effusive component exists. In this setting, port placement can be easily
determined by correlation with axial imaging. In cases where there is significant parietal tumor bulk, it is often best to locate an underlying pocket of fluid first with an 18 gauge spinal needle. Occasionally, tumor burden is such that VATS is impossible and in these instances a small 2 cm incision (again, placed in line with
a potential thoracotomy incision) can easily access the underlying tumor under direct vision. Another merit of VATS is the ability to perform talc pleurodesis. Instillation of 4–5 g of sterile medical grade talc is generally sufficient. Pleurodesis does not impact the ability to perform extrapleural pneumonectomy (EPP) or
pleurectomy/decortication (PD) at a later stage (indeed it can often facilitate dissection), but can offer significant palliation in patients whoare subsequently found not to be surgical candidates. It must be remembered, however, that talc will cause fluorodeoxyglucose (FDG) activity in the pleural distribution and in mediastinal lymph nodes on subsequent positron emission tomography (PET) imaging. For this
reason it is ideal that PET imaging be performed prior to talc pleurodesis. Despite the obvious benefits of VATS as a diagnostic and therapeutic procedure in mesothelioma, it requires general anesthetic and at
least an overnight hospital stay. CT-guided core needle biopsy is a more convenient method of establishing a tissue diagnosis. It has a high accuracy for diagnosis of mesothelioma but is probably less sensitive for determination of true histologic subtype as generally only a single tumor site is biopsied. The incidence of tumor seeding may be also less than with thoracoscopic biopsy [1]. At the University of Texas
M.D. Anderson Cancer Center CT-guided biopsy is the initial method of diagnosis used for patients with suspected mesothelioma. VATS is reserved for patients in whom there is diagnostic uncertainty or for patients in whom treatment of an associated effusion is indicated. extrapleural plane and potential contamination of the incision with tumor. The worst situation occurs when a thoracotomy is performed and a
partial parietal pleurectomy is undertaken in the mistaken belief that “more is better.” In this setting it is virtually impossible to perform an adequate cytoreductive procedure at a later time.
Staging
The American Joint Commission on Cancer (AJCC)/International Mesothelioma InterestGroup (IMIG) staging system is based primarilyon pathologic data. As such it has significant limitations when applied to clinical staging. Many of the factors that contribute tostage designation such as pericardial invasion,
invasion of the endothoracic fascia, lymph node metastases, and diaphragmatic invasion,to name but a few, are simply not possible to determine accurately with current diagnosticimaging techniques. Though PET can identifyoccult distant metastatic disease in up to 25% ofcases, it is insensitive for determining lymph
node involvement or transdiaphragmatic invasion factors that significantly worsen outcome
and generally contraindicate extrapleural pneumonectomy
Laparoscopy
Transdiaphragmatic invasion is a manifestation of advanced disease (Stage IV) and precludes any form of cytoreductive surgery. Involvement may occur either through direct and contiguous invasion of tumor across the diaphragmatic muscle or by lymphatogenous spread via communicating lymphatics between the pleura and the abdomen. This latter form of metastatic spread may lead to peritoneal carcinomatosis
and is not necessarily dependent on the degree of tumor bulk within the hemithorax. Because of the inability of axial imaging (MRI, CT or PET) to accurately differentiate transdiaphragmatic from superficial invasion or tumorabutment, Conlon investigated the use of laparoscopyand identified transdiaphragmatic
invasion in 6 of 12 patients with equivocal CTfindings. Importantly, of the remaining six patients, all underwent thoracotomy and noneas found to have transdiaphragmatic invasion. Based on these findings in 1999 we began routinely performing laparoscopy in patients being considered for extrapleural pneumonectomy. Laparoscopy is performed as an outpatient procedure in combination with ediastinoscopy
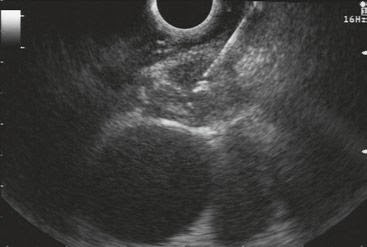
(or, more recently, endobronchial ultrasound (EBUS)), usually utilizing a 10 mm periumbilical port and a 5 mm subcostal port on the same side as the mesothelioma. After initial inspection of both diaphragms and the entire peritoneal cavity the abdomen is irrigated with 1,000 cc normal saline. A 0-degree 5 mm laparoscope
is then placed through the subcostal port and advanced beneath the surface of the saline to closely inspect the underside of the ipsilateral diaphragm. The saline helps surrounding organs (liver, spleen, and omentum) be atraumatically displaced away from the diaphragmatic surface while preserving visibility. Suspicious lesions are biopsied, which generally requires placement of an additional 5 mm port. The lavage
fluid is routinely submitted for cytologic analysis. In 109 patients with potentiallyresectable mesothelioma 9 (8.3%) patients werefound to have transdiaphragmatic extension of tumor, and 1 (0.9%) patient had diffuse peritoneal carcinomatosis. CT scans were suspiciousfor diaphragmatic invasion in only 3 (33%) of these patients. In addition, of 78 patients who underwent peritoneal lavage, 2 (2.6%) patientswere found to have peritoneal micrometastaseswithout obvious diaphragmatic invasion. Thus,
12 (11.0%) patients were identified with unsuspectedabdominal involvement and thus wereable to avoid futile cytoreductive surgery.
Mediastinoscopy
The high prevalence of lymph node metastases in MPM (up to 50% of patients undergoing trimodality
therapy) and the poor prognosis that extrapleural nodal involvement confers, are justifications for preoperative assessment of mediastinal nodal metastases. Unfortunately, current radiographic modalities are inaccurate. The sensitivity of CT for detecting mediastinal N2 disease in mesothelioma is only 50–60% asthere is difficulty in differentiating enlarged mediastinal nodes from adjacent areas of tumor
nodularity. Similarly, PET has relatively lowaccuracy at correctly defining N stage. The efficacy of surgical staging of the mediastinumwith cervical mediastinoscopy (CM) is wellestablished for non-small cell lung cancer; however,the utility of the procedure in mesotheliomais less clear. Schouwink and associates
performed CM in 43 patients with MPM andcompared the staging accuracy of CM with thatof CT scanning. Sensitivity, specificity, andaccuracy were 80%, 100%, and 93%, respectively,for CM compared with 60%, 71%, and67% for CT. Mediastinoscopy failed to identify9 (21%) patients who were found to have positiveintrathoracic nodes at thoracotomy, despite the fact that three of these patients had positive
nodes in sites that were potentially accessibleby CM. We routinely perform mediastinal nodalsampling (now with EBUS) at the time of staginglaparoscopy. We reported use of mediastinoscopyin 62 patients with mesothelioma and identified N2 metastases in 10 (16.1%). Ofthese, 46 underwent extrapleural pneumonectomy.Fourteen (30.4%) patients were found tohave extrapleural (N2) nodes at thoracotomy, of
which CM identified only five preoperatively. The sensitivity and accuracy of CM for detecting N2 disease was only 36% and 80%, respectively. One of the reasons for the low sensitivity is that extrapleural nodal metastases in mesothelioma frequently occur in regions that are inaccessible to mediastinoscopy such as the
internal mammary artery chain, the aortopulmonary window, the anterior mediastnal fat and thymic tissue, the intercostal spaces and the retrocrural and anterior diaphragmatic regions. Combined laparoscopy and mediastinoscopy identified 15 of 118 patients (12.7%) in whom either contralateral nodal disease (N3) or
abdominal involvement precluded further surgical therapy.
Thoracoscopy
More recently, laparoscopy and mediastinoscopy have been combined with bilateral thoracoscopy for surgical staging of patients with mesothelioma. Alvarez et al identified contralateral chest involvement in 3 of 30 (10%) patients and five (20%) were upstaged to stage IV. Additionally, two patients were reclassified rom epithelioid to non-epithelioid histology. Surgical staging identified 26% of patients who would have received no benefit from trimodality therapy. Though experience with bilateral VATS is yet limited, it may have a role in patients who present with a contralateral effusion or noncalcified pleural plaques.
Endoscopic Staging
While generally safe, CM requires a cervical incision and is associated with a small risk of recurrent nerve injury, pneumothorax, tracheal injury, hemorrhage, and even death. Endobronchial ultrasound (EBUS) and esophageal ultrasound (EUS)-guided fine needle aspiration (FNA) of mediastinal lymph nodes have been highly effective for staging non-small cell lung cancer (NSCLC). Since 2006 we
have replaced mediastinoscopy with EBUS forassessment of mediastinal nodes in patients beingconsidered for radical resection of MPM. We compared 50 consecutive patients with mesothelioma who underwent CM with 38patients who underwent EBUS. Sensitivity and negative predictive value for mediastinoscopywere 28% and 49%, and 59% and 57% for EBUS. Furthermore, 11 patients had EUS preoperatively, hich revealed infradiaphragmatic nodal metastases in 5 patients (Fig. 7.4). Tournoy
et al performed EUS and FNA in 32 patients with resumed early stage mesothelioma and identified
N2 metastases in 4 (12.5%) [70]. Of the patients who subsequently underwent extrapleural pneumonectomy and mediastinal node dissection (n = 17) there was only one false negative (4.7%). Mediastinoscopy did not identify additional nodal metastases. The data for EBUS and EUS staging in mesothelioma are preliminary,
however, and further studies will be needed to ascertain their benefit. Though these minimally invasive techniques are safe and less traumatic than mediastinoscopy, there is a risk for false positivity because of the danger of mistaking tumor nodules adjacent to the trachea or esophagus as enlarged lymph nodes. Therefore, the procedure should be performed by an operator skilled in endoscopic ultrasound and familiar
with mesothelioma and only well-defined, circumscribednodes should be biopsied. It is also important that there is evidence of lymphoid tissuein any positive aspirate.
Palliative Surgery
Symptoms in patients with mesothelioma predominately consist of dyspnea, chest pain, cough and constitutional symptoms such asfatigue, fever, and anorexia. Respiratory symptoms are secondary to atelectasis and shunting caused by pleural effusion or lung encasement; or to altered respiratory mechanics secondary tochest wall contraction and impaired movement of the ribs and diaphragm. Surgical palliation is
centered around two issues – treatment and prevention of pleural effusion, and tumor debulkingto allow lung expansion and improved chestwall mechanics.
Pleural Drainage
Treatment of pleural effusion depends on thesize of the effusion, the degree to which it is causing atelectasis and the degree of lung encasement by tumor. Simple thoracentesis israrely effective in providing long-term relief of mesothelioma-related effusion; however, it is areasonable initial procedure to establish a diagnosis
and to evaluate the degree to which thelung will re-expand. In the absence of completere-expansion, pleural symphasis is unlikely tooccur with sclerotherapy. If the lung is trapped because of tumoral involvement of the visceral pleura (as is most often the case except in Stage I disease) placement of an indwelling pleural
catheter such as the PleurX® catherer (CareFusion, San Diego, CA) is preferable. This procedure is most easily performed on an outpatient basis and avoids hospitalization. In addition, complete lung re-expansion is not required to obtain control of the effusion. Tumor progression along the tract of the catheter has
been described but is uncommon. VATS is the preferred method for pleurodesis, particularly in cases where the effusion may be loculated,but will ultimately only be successful in cases where expansion of the majority of thelung can be achieved. In addition to drainage of effusion, VATS provides large quantities of tissuefor diagnosis and histologic subtyping.Limited visceral decortication can occasionally
free entrapped lung, but the case must be taketo limit air leaks as these can lead to the requirement
for prolonged chest tube drainage.
Pleurectomy
Pleurectomy and decortication (PD) have long been used for the control of malignant effusions. The aim of palliative PD is to enable lung re-expansion, ameliorate the contracting effect of tumor on the ribs and intercostal muscles, and to create pleural symphasis. Palliative PD is best accomplished via a posterolateral thoracotomy. Although limited PD can be easily accomplished through a muscle sparing incision, if there is significant tumor burden division of the latissimus dorsi muscle and resection of the seventh rib can greatly facilitate exposure and resection. Dissection is begun by establishing a plane between the involved pleura and the endothoracic fascia. This is most easily accomplished using sharp dissection initially followed by blunt finger dissection. Chest wall bleeding may be controlled using gauze pads for tamponade or use of electrocautery, argon beam coagulation, or radiofrequency such as the highly effective AquaMantys® radiofrequency system (Salient Surgical Technologies, Portsmouth, NH). Once the lung and parietal pleura have been completely mobilized, dissection of the visceral pleura away from the underlying lung parenchyma is performed. The tumor rind is incised on the lateral aspect of the mobilized lung and using sharp dissection a plane is created immediately beneath the visceral pleura. Once established, dissection is continued in all directions using a peanut retractor or using a finger and gauze pad. The pericardium and diaphragmare frequently involved, or at least inseparable from tumor. If palliation is the intent of the procedure rather than cytoreduction, these structures should remain intact, leaving tumor in place where necessary.
7.6
Cytoreductive Surgery
The aim of cytoreductive surgery is to provide a removal of all macroscopic tumor from the hemithorax. It is postulated, though unproven, that R0/R1 cytoreduction may prolong survival in patients particularly those with epithelioid tumors who do not have lymph node metastases. Cytoreductive surgery is usually accomplished in the setting of bi- or tri-modality therapy. Local tumor control appears to be improved with R0/R1 cytoreduction and adjuvant radiation therapy. Because of the high rate of distant recurrences (as
high as 50%), systemic therapy is usually also advisable, though the effect of chemotherapy on reducing distal recurrence is unproven. There are two approaches to cytoreduction: extrapleural pneumonectomy and extended pleurectomy/ decortication (or radical pleurectomy/decortication). Each has its merits as well as limitations and will be discussed separately below.
Extrapleural Pneumonectomy (EPP)
Technique
Extrapleural pneumonectomy involves the enbloc resection of the parietal and visceral pleura, lung, ipsilateral pericardium and diaphragm. Preoperative placement of defibrillator EKG leads is performed in the vent of an Intraoperative rapid supraventricular arrhythmia that requires synchronized cardioversion. Because of the potential risk of injury to the superior vena cava during dissection of rightsided tumors, large bore femoral venous access is obtained. A nasogastric tube is placed, which posterior dissection. A generous posterolateral thoracotomy incision is performed, extending the incision anteriorly in line with the underlying ribs. The latissimus dorsi muscle is divided but the serratus anterior muscle should be spared. In the event of a postoperative bronchopleura fistula, an intact serratus muscle is useful for repair. The anterior most attachments of the muscle should be elevated off the underlying chest wall and retracted superiorly. Removal of the seventh rib provides optimal access to the extrapleural plane, which should initially be developed sharply . Once the correct plane is identified it may be extended in all directions using blunt dissection. It is useful to place gauze packs in areas thathave been dissected to tamponade oozing from the chest wall. We have found the preoperative intravenous administration of tranexamic acid to be useful to control chest wall oozing. The Aquamantys® radiofrequency system (Salient Surgical Technologies, Portsmouth, NH) or an argon beam coagulator is useful for direct control of chest wall bleeding. Once the extrapleuralplane has been dissected to the level of thehilum anteriorly and posteriorly, an incision ismade in the pericardium anterior to the phrenic nerve, and the pericardium attached to the overling pleura and tumor is resected en-bloc with the specimen. Finally, the diaphragm is resected along with the associated overlying lung and tumor. Generally, the diaphragmatic fibers can be bluntly avulsed from their peripheral attachments followed by sharp or cautery dissection of intervening fibers. Once the peripheral attachments are taken down, blunt dissection with sponge forceps allows the muscle to be separated from the underlying peritoneum. It can be difficult to keep the peritoneum entirely intact, especially in the region of the central tendon; however, lacerations inthe peritoneum can be easily repaired with a fine absorbable suture. The unproven rationale for maintaining the integrity of the peritoneumis that it preserves the integrity of the abdominal cavity from potential contamination with tumor from the chest. In the region of the esophageal hiatus, it is ideal to preserve some of the crural fibers to mitigate against herniation of the stomach into the post-pneumonectomy space. Once the entire specimen has been mobilized the hilarstructures can be divided. The pulmonary artery and veins should be divided first. The main bronchus is freed of surrounding tissue to the level of the carina. A firing of the stapling device (generally a TA-30 3.0 mm) is placed on
the distal bronchus first. This allows the anesthesiologist to retract the end of the left-sided double lumen ndotracheal tube back into the rachea while preventing ventilation of the left lung for left-sided tumors. additionally, it prevents migration of bronchial secretions into the chest cavity after division of the main bronchus. The stapling device is then placed across the main stem bronchus at the level of the carina and two separate rows of staples fired before division of the bronchus. Application of the stapler under direct bronchoscopic examination can be useful to ensure that the bronchial stump is flush with the carina and that there is no redundant bronchus left that will retain secretions. Once the specimen is removed from the
chest cavity, hemostasis is secured and the cavity irrigated with at least 3 L of weak betadine solution. The anterior and inferior margins of resection are marked with numerous titanium clips to aid in planning of adjuvant radiotherapy. Though postoperative care is similar to that of any pneumonectomy, certain point are worthy of mention. Early mobilization should be encouraged to lessen the risk of contralateral atelectasis and pneumonia. Transient gastroparesis can occur following EPP, especially where one or both vagus nerves have been injured or sacrificed during dissection, therefore nasogastric drainage should be continued during the first 24 h and great care taken when advancing diet. Because of the greater degree of chest wall oozing and drainage after EPP compared to standard pneumonectomy, it is advisable to leave the chest drain in place for at least 48 h. Earlier withdrawal may allow excessive amounts of fluid to accumulate early in the pneumonectomy space which may cause contralateral mediastinal shift and cardiopulmonary dysfunction. Additionally, excellent control of postoperative pain is required not only for patient comfort but also for optimal respiratory function. Epidural analgesia generally provides better control of pain than intravenous narcotics, and because of the extended thoracotomy incision epidural analgesia should be continued for at least 4–5 days after surgery.
Adjuvant Therapy
Extrapleural pneumonectomy generally provides a more complete cytoreduction compared to radical P/D since the entire lung is removed, limiting the area at risk for local recurrence to the chest wall and mediastinum contiguous with the resected tumor. As the lung is resected, adjuvant radiation may be administered to the postpneumonectomy space. Hemithoracic radiation following P/D is problematic because it is technically difficult to deliver adequate tumoricidal doses of radiation to the entire at-risk area without causing severe toxicity to the underlying lung. Furthermore, conventional photon/electron
beam radiotherapy has not been shown to decrease local recurrence after P/D. EPP is associated with significantly higher postoperative morbidity than P/D, and in most series mortality is also higher (3–8% in experienced centers, . Extrapleural pneumonectomy is usually performed as part of a multimodality therapeutic regimen (Table 7.2). In the absence of adjuvant therapy local recurrence rates range between 30% and 50%. Two recent studies have demonstrated the efficacy of hemithoracic radiation in reducing local recurrence after EPP. In a phase II multicenter study from Memorial Sloan Kettering Cancer Center (MSKCC), Rusch et al delivered 54 Gy of irradiation to 54 patients who had undergone EPP. Radiotherapy was performed using anteroposterior photon beams, placing specially designed blocks over radiation sensitive structures after threshold doses for thoseorgans had been achieved. The corresponding underdosed areas of the chest wall were then treated with matched electron beams. Local recurrences occurred in only 13% and were mainly in the posteroinferior paravertebral sulcus, areas difficult to adequately treat with this radiotherapy technique. Patients with stages I and II had a median survival of 33.8 months whereas the median survival of patients with stage III or IV was only 10 months. A retros ective study, from the M.D. Anderson Cancer Center (MDACC), evaluated 63 patients treated with intensity modulated radiation therapy (IMRT) (median dose 45 Gy) after EPP [52]. IMRT has advantages over conventional radiation because the entire hemithorax can be more accurately targeted while limiting radiation toxicity to surrounding structures. In-field recurrences occurred in only 5% and overall locoregional recurrence was 13%. It should be kept in mind that the patients treated in both these studies were of advanced stage − 69% stage III/IV in the MSKCC study; 87% stage III/IV in the MDACC study. Despite excellent local control, however, distant metastases occurred in 63% and 54% of patients in each study, respectively, suggesting the need for systemic treatment in addition to local therapy. Pleurectomy/Decortication (P/D) The term “pleurectomy/decortication” can mea different things to different surgeons. It can refer to a partial debulking of tumor from the parietal and visceral pleural surfaces leaving large amounts gross tumor behind, it can be a subtotal resection of the parietal and visceral pleura leaving behind only minimal amounts of macroscopic tumor, or it can include complete removal of all macroscopic tumor, which usually entails resection and reconstruction of the diaphragm and pericardium in addition to total pleurectomy . In terms of cytoreductiv surgery, the latter procedure is optimal and is frequently termed “extended” or “radical” pleurectomy/decortication to distinguish it from lesser debulking procedures.
Technique
Radical P/D begins with a complete extrapleural mobilization of the lung to the level of the hilar structures similar to that performed during the initial dissection for EPP. If the pleura/ tumor is inseparable from the pericardium or diaphragm (as it most often is) these structures are resected and reconstructed in a manner similar to that of EPP. Once the lung and overlying pleura have been completely mobilized, an incision is made in the parietal pleura and taken through the tumor and visceral pleura down to the level of the lung parenchyma. Using sharp dissection a plane is created immediately underneath the visceral pleura. This plane is then further elaborated using blunt dissection with a peanut sponge or a gauzed finger. Paradoxically, this is often more easily accomplished in patients who have a significant tumor rind as it can be difficult to completely remove minimally involved pleura. Although the lung parenchyma often bleeds it will usually abate quickly. In this way the entire visceral pleura and overlying tumor and parietal pleura can be resected down to the hilar structures. The pleura is traced all the way into the fissures, and the pulmonary artery and veins will usually be encountered and should be completely freed of any overlying pleura or tumor. Occasionally, lung parenchyma that has been atelectatic for lengthy periods from overlying tumor will seldom expand, and these areas are often best resected with a linear stapler. Similarly, portions of lung that have been devitalized during dissection or those with significant lacerations are often best removed. Though usually all tumor can be resected from the underlying lung, occasionally and in particular in early stage disease, there can be a multitude of tiny subpleural tumor deposits that remain adherent to the lung after visceral pleurectomy. These may be directly removed using sharp dissection or may be ablated using thermal energy (argon beam , electrocautery, radiofrequency ablation, or cryoablation (personal observation). Typically, there are three large-bore chest drains : one over the diaphragm coursing posteriorly to drain the costovertebral recess, one in the posterior sulcus,
and one anteriorly.
Postoperative Care
Because the chest wall can continue to slowly ooze blood and maximum expansion of the lung is ideal postoperatively, it can be helpful to keep patients intubated overnight following pleurectomy/ decortications. This ensures maximal expansion of atelectatic lung and the inflated lung aids in tamponading diffuse chest wall
oozing. Air leaks are prominent, particularly on positive pressure ventilation, but will usually subside within a week. Chest drains are placed at the lowest amount of suction that is sufficient to maintain complete expansion of the lung, usually negative 10–20 cm H20.
Adjuvant Therapy
Because the lung is left in situ, P/D offers less complete cytoreduction than EPP but impacts pulmonary function significantly less. This is reflected in the lower perioperative mortality reported in most series compared to EPP , and also in the higher incidence of local recurrence, which generally ranges from 50% to 100% . Unlike EPP, the intact lung that remains limits the ability to administer effective radiation postoperatively. Gupta et al reported 123 patients who received hemithoracic radiation therapy (median 43 Gy) similar to the regimen used at MSKCC for EPP. Despite a preponderance of patients with stage I and II (59%) median survival was only 14 months, and local recurrence occurred in 56% of patients. Similarly, Lee and colleagues performed P/D on 26 patients using intraoperative radiation followed by postoperative 3-dimensional conformal radiation or IMRT. 69% of patients had stage I disease and so it is not surprising that the median survival was reasonably good (18 months). Fifty percent of patients had recurred or died by 1 year however, and although the exact frequency of local recurrences was not reported, the author stated that most patients died from progressive disease, and that the “site of f ilure was mostly locoregional.”
Intrapleural Therapies
The relatively high local recurrence rate following cytoreductive surgery alone has prompted use intrapleural therapies after PD or EPP. These have primarily involved intrapleural administration of platinum-based chemotherapy or intracavitary photodynamic therapy (PDT) with preoperatively administered photosensitizers. The concept behind intrapleural therapy is straightforward – extrapleural dissection
of mesothelioma cannot reliably achieve an R0 resection and microscopic tumor deposits are frequently left behind. This is evident in local recurrence rates of up to 30–50% following EPP alone. Because of the even greater propensity for microscopic, and even macroscopic tumor remnants following pleurectomy/decortication, local recurrence rates can be as high as 70–100% with this procedure. Intrapleural chemotherapy is theoretically able to treat the entire at-risk area of the hemithorax and has been shown to permeate up to 5 mm into tissue. Most trials of ip chemotherapy however have been small phase I and II studies with limited numbers of patients. Rates of local recurrence have varied between 17% and 100% . Earlier studies tended to rely on the instillation of chemotherapeutic agent into the chest cavity via chest drains in the postoperative period. More recently, capitalizing on the tumoricidal effect of hyperthermia, investigators have evaluated intraoperative intrapleural perfusion of cytotoxics heated to 42°C. The largest study of this nature was recently reported by Tilleman and colleagues from the Brigham and Women’s Hospital. Ninety-two patients were enrolled on a phase II study which included EPP and intraoperative heated chemoperfusion with cisplatin. Renal function was maintained by the concomitant administration of sodium thiosulfate and amifostine. Though recurrence within the ipsilateral chest was low (17%) and operative mortality 4%, median survival was only 13 months. Admittedly, nearly half of the patients had stage III disease and 42% had non-epithelioid histology. Thirty-two percent recurred in the contralateral chest and 26% in the abdomen, highlighting the need for more effective systemic therapies. The same group previously published their experience using a similar regimen in 44 patients who were ineligible for EPP and who underwent PD instead. Local recurrence was 57% and treatment related mortality was 11%, probably at least somewhat related to the fact that this was an older, higher risk group.
Extrapleural Pneumonectomy Versus Pleurectomy/Decortication There is considerable controversy over the selection of which operation is the most appropriate. Some surgeons perform only EPP, others only P/D, and many tailor selection of operation to the patient and the degree of tumor load. As previously mentioned, in addition to the oncologic pros and cons of either operation, selection must also take into account the application of adjuvant therapies as well as patient and tumorrelated factors. Clearly, an elderly patient or one with poor cardiopulmonary function is unlikely to tolerate EPP and would be better served with P/D. Patients with non-epithelioid histology (especially sarcomatoid) have poor outcome after EPP and these patients should also probably undergo P/D if surgery is even contemplated at all. The controversy exists mainly around good performance status patients with epithelioid tumors in whom either operation would be technically feasible. There have been no randomized prospective comparisons of these procedures in carefully staged and stratified patients. The largest retrospective comparison of EPP and P/D that exists was performed by Flores and colleagues who reported a combined series from three separate institutions that included 663 patients. Overall median survival was 14 months and was slightly longer for the 278 patients who underwent P/D than for the 385 patients who had EPP (16 vs 12 months, p<0.001). However, it should be recognized that significantly more patients in the P/D/ group had early stage tumors (35% vs 25% (p < 0.001)). In addition, the institutions involved in this study performed P/D not only for patients who would not medically tolerate EPP, but also for fit patients when there was “minimal visceral involvement” [23] and for patients with low tumor volume [46]. This bias toward performing P/D on patients with biologically more favorable tumors makes it difficult to draw firm conclusions from the data. Furthermore, a previous analysis from one of the institutions revealed no difference in survival among 222 patients with EPP and 126 patients with P/D